PSM files comments on HHS's proposed Canadian drug importation rules; cites danger to patients
 Today The Partnership for Safe Medicines filed comments with the Department of Health and Human Services (HHS) about the dangers posed by its draft regulations for state programs which would import medicine from Canada. The comments:
Today The Partnership for Safe Medicines filed comments with the Department of Health and Human Services (HHS) about the dangers posed by its draft regulations for state programs which would import medicine from Canada. The comments:
- cite historic problems with and patient harm from Canadian vendors selling counterfeit cancer and other medications to the U.S.;
- show broad opposition to the plan by Canadian stakeholders; and
- provide significant, proven solutions for reducing drug costs that don't impact patient safety.
Read PSM's comments below, or in PDF format. We encourage you to file your own response using our comment portal. Finally, you can read our one page summary of the problems with the HHS plans to help you compose your own comments to HHS.
Resources:
Our short one-pager outlines the reasons why Canadian drug importation won't work. Use it when filing your own comments with HHS about why there are better, proven ways to reduce drug prices.
PSM's comment on the Department of Health and Human Services' proposed rule for the Importation of Prescription Drugs:
February 11, 2020
As a non-profit that has been working to protect patients from counterfeit and substandard medicines for more than a decade, The Partnership for Safe Medicines is concerned that Department of Health and Human Services’ proposed rule for the importation of prescription drugs does not protect patients from the threat of unreliable and counterfeit medicine.
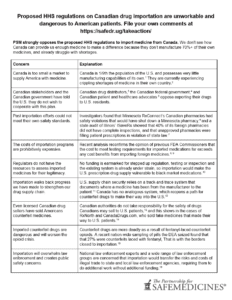
THE PROPOSED RULE WOULD ENDANGER PATIENT SAFETY
The proposed rule breaks the track and trace system outlined in the Drug Supply Chain Security Act (DSCSA), which was passed in 2013 to protect patients from fake medicines that had made their way into our drug supply. When the DSCSA is fully enacted, every package of prescription medicine sold in the U.S. will have a secure electronic record listing every entity involved from the moment it is manufactured until the moment it reaches a patient. This system will allow U.S. regulators and supply chain entities to track prescription drugs through the distribution system, helping to ensure against counterfeit medicines and protecting the public health. Because Canada does not have a compatible system, any importation program would rely on waiving track and trace requirements for imported drugs, as HHS/FDA proposes. Doing so would re-open a path for black market drug sellers to substitute cheaper counterfeit and unsafe drugs into the U.S. supply chain before they enter our own track and trace system.
The proposed rule relies on Canadian licensing to validate the legitimacy of foreign sellers, but licensed Canadian drug sellers have sold Americans counterfeits in the past. Canadian authorities have been explicit that they cannot take responsibility for the safety of drugs that Canadians may sell to U.S. patients. As Diane Gorman, then Assistant Deputy Minister of Health Canada, put it in 2004, “Health Canada does not assure that products being sold to U.S. citizens are safe, effective, and of high quality, and does not intend to do so in the future.” Gorman spoke truthfully: as noted below, licensed Canadian sellers like Andrew Strempler and CanadaDrugs.com have sold U.S. patients and medical practices counterfeit medicines.
THE PROPOSED RULE WOULD NOT RESULT IN A SIGNIFICANT REDUCTION IN THE COST OF PRESCRIPTION DRUGS TO THE AMERICAN CONSUMER
There is no guarantee of savings for consumers who participate in these programs. The proposed rule has no assessment of whether importation would “result in a significant reduction in the cost of covered products to the American consumer,” as required under law. Experts from the London School of Economics have studied parallel trade of medication in Europe across country borders and found that savings are usually consumed by middle men in the supply chain instead of being passed on to consumers.
Past state-administered drug importation experiments were not safe and did not save money. States that experimented with importation between 2003 and 2009 ran into trouble running safe programs. In 2004, inspectors found Minnesota’s Canadian pharmacies had safety violations that would have shut down any pharmacy in Minnesota: they asked pharmacists to approve 100 new prescriptions or 300 refill prescriptions per hour; shipped medicine that required refrigeration without it; failed to label medicine properly; and dispensed grossly improper amounts of medications. Despite these threats to public health, the program continued until 2010, when the state determined that it was not saving money.
Illinois’ ISaveRx, which grew to include Kansas, Wisconsin, Vermont and Missouri, had similar safety and public health issues: a 2006 audit found that 40% of required inspections of the foreign pharmacies were never completed and pharmacies that had not been approved were filling prescriptions anyway, in violation of state law.
The costs of importation programs are prohibitively expensive. The Medicare Modernization Act of 2003 (MMA) requires that documentation show that “each batch of the [imported] prescription drug in a shipment was statistically sampled for authenticity and degradation.” In a recent analysis, Dr. Kristina Acri, a professor at Colorado College’s Department of Economics & Business, examined testing costs for drugs which could be imported from Canada, and concluded that the cost to meet the MMA’s testing requirements would far exceed any cost benefits from importing foreign medicines. Dr. Acri also examined the potential costs of treatment failure because of substandard medicine, and the cost of treating an adverse medical event. She concluded that “Pharmaceutical importation plans are politically attractive, but the numbers demonstrate that they fail to deliver cost savings.” Acri’s opinion is not unique. In March 2017, four former FDA Commissioners also argued that importation “will not achieve the aim, and...is likely to harm patients and consumers.”
THE PROPOSAL FURTHER RISKS AMERICANS’ WELL-BEING
State boards of pharmacy and departments of health have no ability to regulate foreign sellers. State attorneys general cannot compel foreign sellers to appear in court. If a Canadian seller did provide fake drugs to state wholesalers or pharmacies, that state’s regulators and law enforcement have little recourse. State regulators can demand that a U.S. wholesaler provide records and open its doors to inspection, and if they refuse to provide information, a regulator can cite them or revoke their license. State inspectors do not have the same rights over a Canadian vendor, who could hide records from them and resist inspections without incurring legal danger. Furthermore, a state can write as many requirements as they want into their drug importation plan, but Canadian companies are not legally required to abide by those rules. If a state determined that it should prosecute a Canadian drug seller for a crime, it lacks the legal authority the federal government has to ask Canada to extradite those responsible.
The rule relies on stepped up review by overwhelmed regulators in each state or other entity serving as a SIP sponsor. State boards of pharmacy already lack sufficient inspectors to be able to adequately inspect wholesalers in other states, and rely on mutual license recognition, hoping that that is safe enough. Law enforcement and regulators are already struggling to inspect large volumes of pharmaceuticals coming over the U.S. border, including deadly fentanyl and other drugs masquerading as legitimate medicine.
These resource-strapped regulators will not have the ability to oversee an importation program under the proposed rule and would not be able to protect the public health. Moreover, a state importation program would stretch resources even more, exacerbating risks already posed by counterfeit medicines.
COSTLY IMPLEMENTATION REQUIREMENTS AND THE DISPARITY BETWEEN U.S. AND CANADIAN MARKETS MAKE THE RULE UNWORKABLE
Prosecuting overseas drug sellers for counterfeit drug crime is very expensive, time consuming, and challenging and does not guarantee justice for victims. Prosecutions that require extradition of foreign citizens are resource-intensive, and foreign drug counterfeiters often receive light sentences or no sentences at all. For example:
- Licensed Canadian pharmacist Andrew Strempler, sold Americans prescription drugs—some counterfeit—that he falsely marketed as Canadian, and avoided an outstanding U.S. warrant by living in Panama. When the U.S. finally got hold of him, he pleaded guilty and was sentenced to four years in prison, but only spent two and a half years behind bars.
- When subsidiaries of CanadaDrugs.com sold American medical practices $78 million in non-FDA approved drugs, some of which were counterfeit, the cases ended in 2018 plea deals. CEO Kris Thorkelson served a six-month house arrest followed by probation and a small fine.
These prosecutions underscore the threat posed to the American public health by foreign bad actors. The proposed rule would undermine the existing supply chain and create opportunities for these bad actors to exploit.
The proposed rule would exacerbate risks posed by transshipments and counterfeits from or through Canada. Drug importation would increase the threat of illegitimate products entering the US. As former FBI Director Louis Freeh noted in a 2017 report, “drug importation would increase incentives for individuals and criminal organizations to transship products through Canada that are likely to be counterfeit, diverted, adulterated, sub-standard and/or other non-FDA approved products.”
The proposed rule could lead to drug shortages in Canada, harming Canadian public health. Canada already suffers from significant drug shortages—more than 2000 medicines are in shortage today. The effect of those drug shortages on Canadian residents is substantial: A Canadian Pharmacists Association survey in November 2018 revealed that 25% of Canadians had personally experienced or known someone who had experienced a drug shortage in the last three years. As Kirsten Hillman, Canada’s Acting Ambassador to the United States, pointed out in November 2019, Canada consumes only two percent of the global drug supply, while the United States consumes 44 percent. Moreover, at 329.45 million in 2019, the U.S. population is nearly nine times larger than Canada’s. That huge difference means that Canada’s prescription drug supply would last less than six months if importers sourced just 20% of U.S. prescriptions from Canadian wholesalers. Regardless of how carefully states design their importation plans, these numbers make it clear that Canadian vendors would have no way to supply U.S. patients without turning to medicines that were not approved or earmarked for Canadian citizens. Canadians seem to know this: Canadian drug distributors, the Canadian federal government, and Canadian patient and healthcare advocates oppose exporting their drugs to U.S. residents.
IT IS CLEAR AT THIS JUNCTION THAT THE STRUCTURAL SAFETY RISKS AND OTHER CONCERNS MEAN THAT HHS SHOULD NOT MOVE FORWARD WITH THIS PROPOSED RULE. INSTEAD, PSM ENCOURAGES HHS TO CONSIDER OTHER PROVEN SOLUTIONS TO BRING PATIENTS FINANCIAL RELIEF AT THE PHARMACY COUNTER.
Provide more resources to the FDA so that it can more quickly review new generic medicines and biosimilars. Data compiled and published by the U.S. Food and Drug Administration show that greater competition among generic drug makers is associated with lower drug prices.
As medicine becomes more complex, regulatory review to establish equivalence requires additional resources and expertise. Generics are a proven way to reduce drug costs for the American consumer and unlike Canadian drug importation, they scale up for all of America. We should be investing in the acceleration of generic drug application reviews, not policy unicorns such as drug importation.
Regulate middlemen with predatory pricing practices such as pharmacy benefit managers. Over and over again, in state after state, we’ve seen policy analysts dig down to find out what’s driving prices for consumers after medicine leaves the factory floor and the answer is often found in middlemen such as pharmacy benefit managers who claim they are using their buying power to achieve economies of scale. In reality, pricing transparency reveals that they are making enormous profits marking up medicine as its sale passes between manufacturers, wholesalers, dispensing pharmacists, and patients.
- A New York State Senate report declared that “PBMs often employ controversial utilization and management tools to generate revenue for themselves in a way that is detrimental to health plan sponsors, patients, and pharmacies.”
- In an outside actuarial study, West Virginia estimated $54,450,000 in savings to the West Virginia Medicaid program after removing the PBM sponsored managed care and replacing it with a fee-for-service model relying on local in-state pharmacies.
- In an Ohio Auditor General’s report, it was found that PBMs pocketed $208mm in fees on generic drugs in a single one year period, despite the fact that generic medicine is a significant driver of cost savings for American patients.
Foster new pricing models. New and novel methods of paying for healthcare are gaining ground and when implemented, showing significant savings without sacrificing safety. These flat-fee agreements are in place in Australia, and in several U.S. states and they are showing promise.
- “The ‘Netflix’ model for hepatitis C drugs is saving Australia a lot of money.”
- A Boston Consulting Group analysis says Netflix-style pricing would save average EU countries $3.2bn over 10 years because of savings related to early cures.
- “Washington state becomes the latest to embrace a Netflix model for buying hep C drugs.”
Conclusion
PSM strongly encourages the Administration to withdraw this deeply flawed rule, as it would significantly increase the risk to the public health of receiving counterfeit, adulterated, misbranded, or otherwise unsafe medicines. Solutions to the challenge of healthcare costs in America that do not sacrifice safety exist, if we only have the courage to implement them.